Insulin Resistance – What You Need to Know
What Is Insulin Resistance?
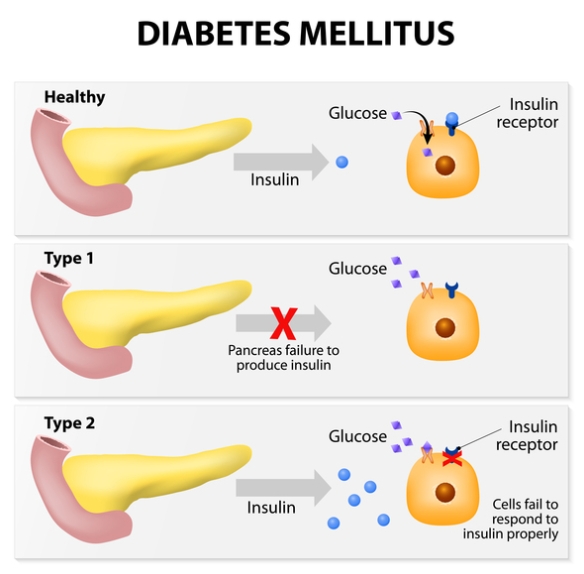
Insulin resistance is a metabolic condition where the body’s cells become less responsive to the hormone insulin. Insulin, produced by the pancreas, is vital for converting glucose (sugar) into energy, allowing cells to utilize blood sugar as fuel. When cells do not respond effectively to insulin, the body requires more of the hormone to achieve the same effect, leading to higher insulin levels in the blood. Over time, this can result in various health complications, including type 2 diabetes and cardiovascular disease.
Insulin Resistance Symptoms
Identifying insulin resistance can be challenging, as symptoms may be subtle. Common signs include:
- Increased Hunger: Cells are not absorbing glucose, leading to constant cravings for food.
- Fatigue: Inefficient glucose utilization can cause energy depletion.
- Weight Gain: Particularly around the abdomen, due to hormonal imbalances.
- Difficulty Concentrating: Also known as “brain fog,” owing to fluctuating blood sugar levels.
- Darkened Skin: Acanthosis nigricans, characterized by dark patches, often appears on the neck or armpits.
- High Blood Pressure: Insulin resistance can lead to increased blood pressure levels.
- Elevated Blood Sugar Levels: Regularly high sugar levels are a strong indicator of insulin resistance.
Early identification of these symptoms can lead to more effective management and a decrease in the risk of further complications.
What Causes Insulin Resistance?
Several factors contribute to the development of insulin resistance, including:
- Obesity: Excess fat, especially visceral fat around the abdomen, can disrupt insulin signaling.
- Physical Inactivity: Lack of exercise can hinder glucose uptake by muscle cells, increasing insulin resistance.
- Genetics: A family history of type 2 diabetes may elevate an individual’s risk for insulin resistance.
- Hormonal Changes: Conditions like polycystic ovary syndrome (PCOS) can influence insulin sensitivity.
- Diet: Diets high in processed foods, sugars, and unhealthy fats can contribute to insulin resistance.
- Sleep Deprivation: Poor sleep can lead to hormonal changes that adversely affect insulin sensitivity.
Recognizing these risk factors is crucial in taking proactive steps toward better health.
Insulin Resistance Diagnosis
Diagnosing insulin resistance typically involves a combination of symptom assessment and laboratory tests. Common diagnostic methods include:
- Fasting Blood Sugar Test: Measures blood sugar after fasting for at least 8 hours. Levels above 100 mg/dL may indicate insulin resistance.
- Hemoglobin A1c Test: Provides an average blood sugar level over the past three months. A result above 5.7% indicates prediabetes.
- Oral Glucose Tolerance Test (OGTT): Measures blood sugar before and after consuming a sugary drink. It assesses how well the body processes glucose.
- Insulin Levels Measurement: High fasting insulin levels may indicate insulin resistance.
Early diagnosis facilitates timely interventions and reduces the risk of progression to more severe conditions.
How Insulin Resistance Progresses to Type 2 Diabetes
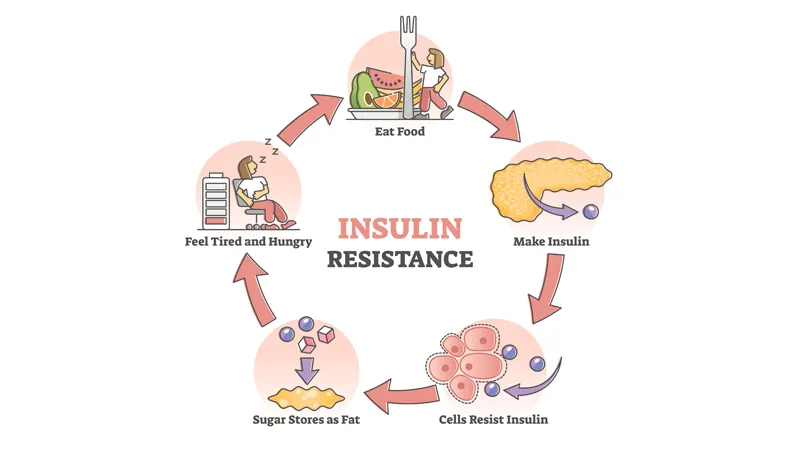
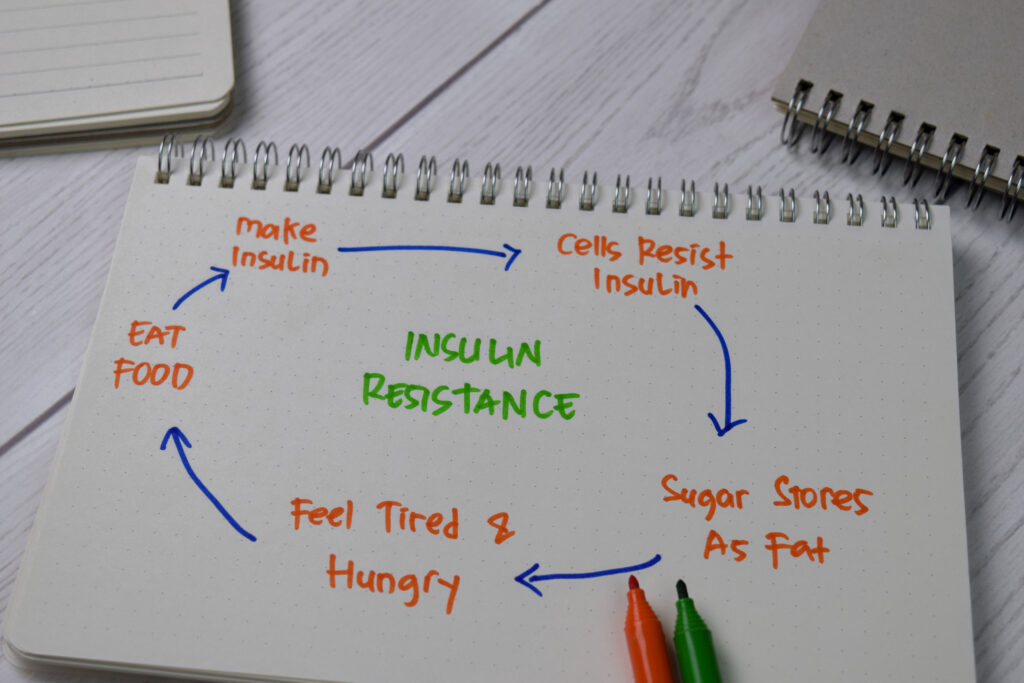
Insulin resistance does not lead to diabetes overnight. The progression typically follows this trajectory:
- Insulin Resistance: Cells become less responsive to insulin, resulting in higher insulin production.
- Increased Blood Sugar Levels: As insulin effectiveness decreases, glucose levels begin to rise in the bloodstream.
- Pancreatic Strain: The pancreas over-exerts itself to produce more insulin to manage rising blood sugar levels.
- Beta Cell Dysfunction: Over time, the pancreatic beta cells that produce insulin may become exhausted and dysfunctional.
- Type 2 Diabetes: Eventually, the pancreas can no longer keep up with insulin demands, leading to consistent high blood sugar levels and a diagnosis of type 2 diabetes.
Understanding this progression highlights the importance of addressing insulin resistance early to prevent further complications and diabetes.
Insulin Resistance Treatment
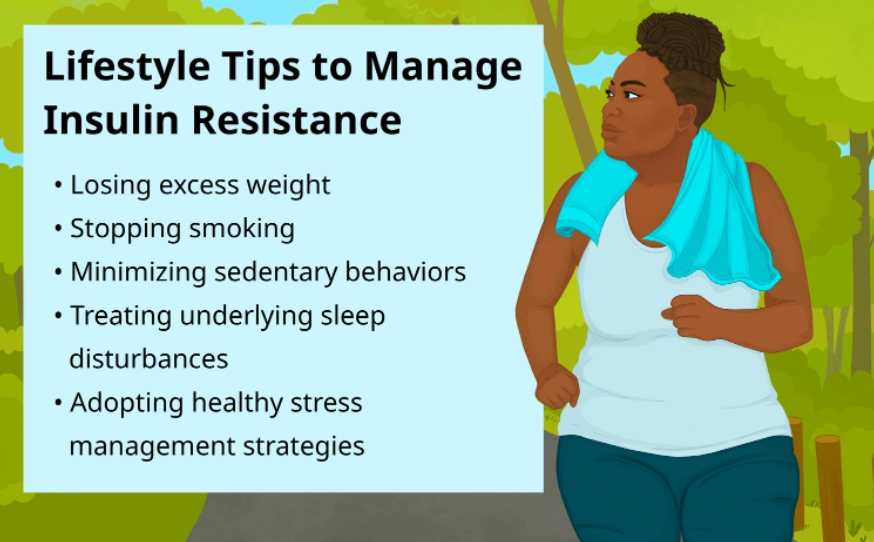
Treating insulin resistance is achievable through lifestyle changes and, when necessary, medical intervention. Key strategies include:
- Dietary Changes: Focus on whole, unprocessed foods rich in fiber, including fruits, vegetables, whole grains, lean proteins, and healthy fats. Reducing sugar and refined carbohydrate intake is essential.
- Regular Exercise: Engaging in at least 150 minutes of moderate aerobic activity per week can significantly enhance insulin sensitivity.
- Weight Management: Losing even a modest amount of weight can enhance insulin sensitivity and reduce associated health risks.
- Medications: In some cases, healthcare providers may prescribe medications like metformin to enhance insulin sensitivity.
- Monitoring: Regularly tracking blood sugar levels and working with healthcare professionals for personalized management helps in achieving optimal outcomes.
Creating a tailored intervention plan can lead to significant improvements in health outcomes and reduce the risk of type 2 diabetes.
Insulin Resistance Complications
If left unaddressed, insulin resistance can lead to several severe complications, such as:
- Type 2 Diabetes: As mentioned, insulin resistance is a precursor to diabetes.
- Heart Disease: Insulin resistance is associated with increased risks for heart conditions, including high blood pressure, high cholesterol, and atherosclerosis.
- Kidney Damage: Diabetes can lead to diabetic nephropathy, potentially resulting in kidney failure.
- Vision Problems: Diabetic retinopathy, stemming from unmanaged blood sugar levels, can lead to vision loss.
- Nerve Damage: Peripheral neuropathy can occur, leading to pain and tingling in extremities.
- Metabolic Syndrome: A cluster of conditions, such as elevated blood pressure and cholesterol levels, increases the risk of heart disease.
Understanding the complications underscores the urgency of addressing insulin resistance through lifestyle modifications and monitoring.
Living With Insulin Resistance
Living with insulin resistance requires a proactive approach that emphasizes health and wellness. Here are essential strategies:
- Education: Understanding insulin resistance, its implications, and management strategies empowers individuals to take charge of their health.
- Support System: Connecting with healthcare providers, support groups, or family can provide motivation and accountability.
- Healthy Habits: Establishing regular habits around diet, exercise, and sleep is vital for maintaining health.
- Stress Management: Practicing stress-reducing techniques like mindfulness, yoga, or meditation can improve overall well-being and insulin sensitivity.
- Regular Check-Ups: Frequent consultations with healthcare professionals can facilitate ongoing monitoring and adjustments to management strategies.
Insulin resistance is a critical health concern that requires attention and action. By understanding its symptoms, causes, and potential complications, individuals can take proactive steps to manage their health. A focus on diet, exercise, and regular monitoring plays a vital role in reversing insulin resistance and reducing the risk of severe complications, including type 2 diabetes. Knowledge, empowerment, and commitment to a healthier lifestyle can lead to significant improvements in health and overall quality of life.
Taking charge of your health means addressing insulin resistance today. Start your journey toward a healthier future by making informed choices and seeking support from healthcare professionals. You have the power to create positive change—don’t wait until it’s too late!



