Diabetes Insipidus vs. Diabetes Mellitus: What Are the Differences?
What Is Diabetes Insipidus?
Diabetes Insipidus (DI) is a rare condition that affects the body’s ability to regulate water intake, leading to excessive thirst and the production of large volumes of dilute urine. Unlike diabetes mellitus, DI is not related to blood sugar levels or insulin. It occurs due to an insufficient secretion of the anti-diuretic hormone (ADH), also known as vasopressin. The condition can be classified into two main types: central diabetes insipidus and nephrogenic diabetes insipidus.
Central DI is caused by damage to the pituitary gland, which results in insufficient ADH release. Nephrogenic DI occurs when the kidneys do not respond properly to ADH. The causes may vary, including genetic factors, head trauma, certain medications, or underlying health conditions. The primary symptoms revolve around excessive urination and thirst, leading to potential dehydration if not addressed properly.
What Are the Differences?
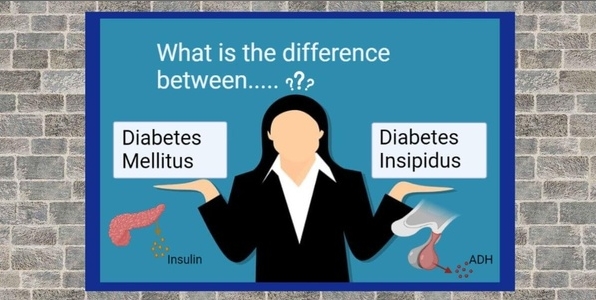
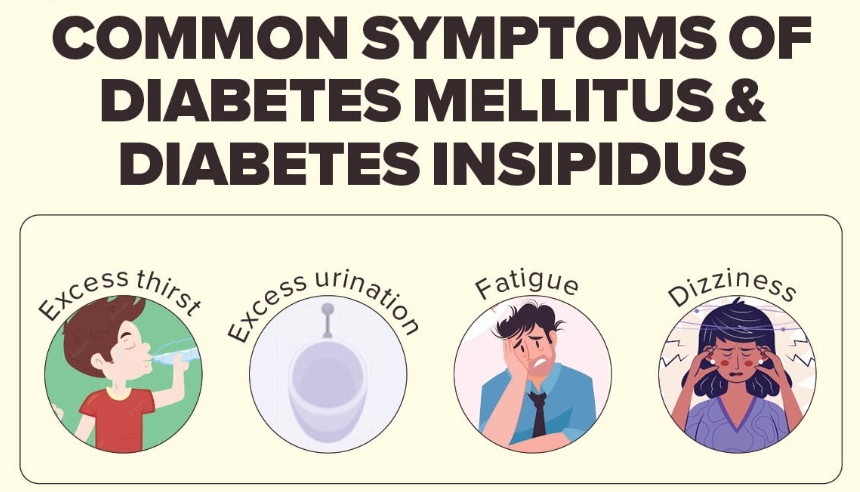
While both diabetes insipidus and diabetes mellitus share a part of their name and result in excessive thirst and urination, they are fundamentally different conditions.
Diabetes Insipidus:
- Hormonal Disorder: Results from a deficiency or resistance to ADH.
- Urine Composition: Produces large amounts of dilute urine.
- Blood Sugar Levels: Does not affect blood sugar levels.
- Management: Often involves desmopressin (a synthetic form of ADH) or specific dietary modifications.
Diabetes Mellitus:
- Metabolic Disorder: Involves issues with insulin production or function.
- Urine Composition: May produce concentrated urine but can also result in glucose in urine due to high blood sugar.
- Blood Sugar Levels: Directly impacts blood sugar levels, leading to hyperglycemia or hypoglycemia.
- Management: Requires lifestyle changes, monitoring blood sugar, insulin therapy, or oral medications.
Causes of Diabetes Insipidus vs. Diabetes Mellitus
Understanding the underlying causes of these conditions is crucial for effective management.
Causes of Diabetes Insipidus:
1.Central Diabetes Insipidus:
- Damage to the pituitary gland from surgery, injury, or tumors.
- Autoimmune disorders.
- Infections affecting the brain.
2.Nephrogenic Diabetes Insipidus:
- Genetic mutations affecting kidney function.
- Chronic kidney disease.
- Medications, such as lithium.
Causes of Diabetes Mellitus:
- Autoimmune destruction of insulin-producing beta cells in the pancreas.
- Genetic predisposition.
Type 2 Diabetes:
- Insulin resistance due to obesity, age, and lifestyle factors.
- Genetic factors and family history.
Type 3 Gestational Diabetes:
- Hormonal changes during pregnancy leading to insulin resistance.
Recognizing the symptoms helps in timely diagnosis and treatment.
Symptoms of Diabetes Insipidus:
- Excessive Thirst: Intense thirst that persists despite fluid intake.
- Frequent Urination: Production of large volumes of urine (up to 20 liters per day).
- Nocturia: Frequent urination at night, disturbing sleep.
- Dehydration: Possible symptoms include dry mouth, skin, and fatigue if water intake is insufficient.
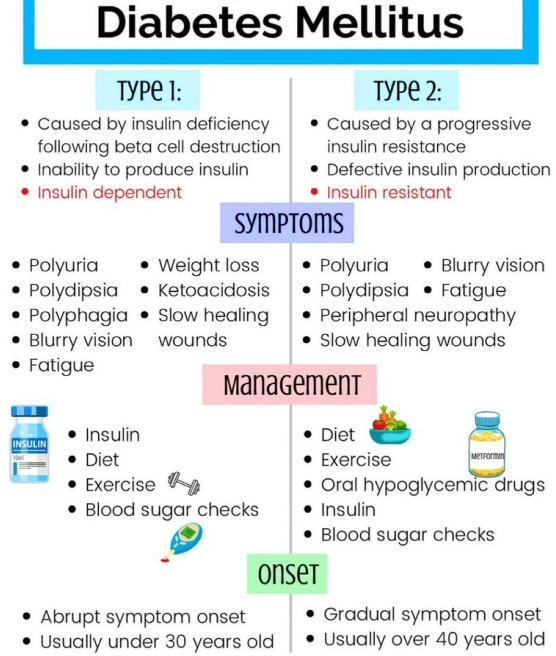
Symptoms of Diabetes Mellitus:
- Increased Thirst: Frequent thirst, often accompanied by dry mouth.
- Frequent Urination: More frequent urination than normal, especially at night.
- Fatigue: Feeling unusually tired and weak.
- Unexplained Weight Loss: Particularly in Type 1 diabetes due to the body using muscle and fat for energy.
- Blurry Vision: Changes in vision due to fluid changes in the lenses.
Proper diagnosis ensures appropriate treatment.
Diagnosing Diabetes Insipidus:
- Medical History: Discussing symptoms and any relevant medical history.
- Water Deprivation Test: Monitoring the body’s response to withheld fluids.
- Urine Tests: Analyzing urine concentration and output.
- MRI Scan: Imaging to check for abnormalities in the pituitary gland.
Diagnosing Diabetes Mellitus:
- Blood Tests: Checking fasting blood sugar levels, A1c tests, and glucose tolerance tests.
- Urine Tests: Testing for glucose and ketones in urine.
- Medical History: Evaluation of symptoms and family history.
Treating Diabetes Insipidus vs. Diabetes Mellitus
Effective treatment approaches vary significantly for each condition.
Treating Diabetes Insipidus:
1.Medications:
- Desmopressin: Used to replace ADH for those with central DI.
- Thiazide Diuretics: In some cases of nephrogenic DI, they may paradoxically reduce urine output.
2.Lifestyle Modifications:
- Increased fluid intake to prevent dehydration.
- Monitoring symptoms closely.
Treating Diabetes Mellitus:
Type 1 Diabetes:
- Insulin Therapy: Necessary for managing blood sugar levels.
- Blood Sugar Monitoring: Regular testing to adjust insulin dosages.
Type 2 Diabetes:
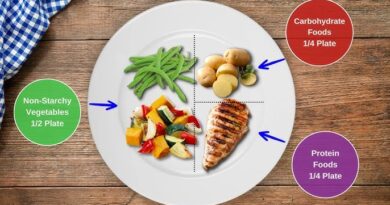
- Lifestyle Changes: Promoting a healthy diet and regular exercise.
- Oral Medications: Prescribing medications to help manage blood sugar.
- Insulin Therapy: May be necessary as the condition progresses.
Diabetes Insipidus and Diabetes Mellitus may share some symptoms but are distinct conditions with different causes, management strategies, and implications for health. Understanding these differences can empower individuals to seek appropriate care and make informed health decisions.
If you experience symptoms related to either condition, consult a healthcare provider for accurate diagnosis and treatment tailored to your specific needs. Early intervention can lead to better health outcomes and improve your quality of life. Stay informed, stay hydrated, and take control of your health today!
This guide aims to raise awareness of the differences and similarities between Diabetes Insipidus and Diabetes Mellitus. Recognition of symptoms and understanding of treatment options are crucial in managing these conditions effectively. Please ensure to continue the dialogue with healthcare professionals for robust health management strategies.